Our measures of success
We’ve applied the same surgery consecutively for 35 years to correct more than 2,500 cases of all severities and for patients of all ages. There has been no need to cut bones or fuse joints. Almost all other corrective surgeries have done otherwise.
Traditionally, surgeons use a deformity severity scale to determine their choice of surgical treatment. A hallux valgus deformity is graded as mild, moderate, severe or extreme depending on the degree in displacement of affected bones. But underneath, they share the same pathology, and hypothetically, should be corrected by the same surgery, only with rare exceptions. Syndesmosis Surgery is perhaps the only procedure that does not discriminate since it equally addresses their common pathology.
Many bunion feet eventually develop secondary problems such as painful calluses, flexible clawed toes, bunionettes, and even knee or back pain as the primary deformity starts to compromise the normal mechanical function of the foot for walking. Therefore, holding to the same principle, if the deformity can be truly corrected and normal foot function restored, then these problems will be free from their cause and resolved automatically without additional surgeries. Following Syndesmosis Surgery, we’ve regularly observed the disappearance of these secondary problems.
We have also applied the same Syndesmosis Surgery principle to salvage a number of recurrent cases after bone-breaking (osteotomy) and even joint-fusion (Lapidus) procedures.

To us, surgical success is a foot capable of returning to unrestricted activities and shoes without pain or recurrence.
Full-function recovery as told by our patients
The very definition of ‘success’ is subjective, and it can also have different meanings to surgeons and patients. While surgeons may be satisfied by the straightness of the big toe, patients are also interested in the full-function recovery of their feet.
In our opinion, if a patient still has pain after 6 weeks, the surgery was not so successful. If a patient is still not able to run or wear high heels after 6 months, the surgery was not so successful. If the condition recurs, even after 10 years, the surgery was not so successful.
We believe the highest standard of success is usually told by patients themselves. That’s why our most powerful evidence is found in the compelling stories directly from our patients.
Function versus Appearance
Often corrective surgery outcome reports are focused on the angle measurements of the bones in isolation and not enough on the correlation between the foot’s functional results and their bone re-alignment.
We regard the improvement of a foot’s appearance as a cosmetic result that is simply a by-product of Syndesmosis Surgery. The Procedure’s quantifiable success lies in its ability to restore function that is verifiable with an objective test method. After all, the human foot is primarily for function, not for show.
Is there a way to measure foot function?
Being able to walk is not a true evaluation of the foot’s functional ability. To be objective and comparable, there are several computerized devices to assess the real-time pressure distribution of a foot against the ground while walking. The distribution pattern can also be quantified to demonstrate any true functional improvement after surgery.
We’ve used F-Scan® for more than 10 years to verify the function outcomes after Syndesmosis Surgery. The biomedical engineering department of Hong Kong’s Polytechnic University has analysed our results, confirming Syndesmosis Surgery could significantly and consistently improve the function of big toe and the foot.
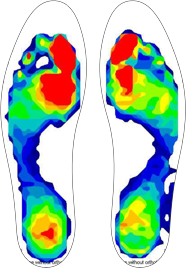
Normal Foot F-Scan
The inner foot carries most of the body weight and contributes up to 80% of the power required for normal walking. A function scan of a normal gait shows the most force under the big toe side of foot.
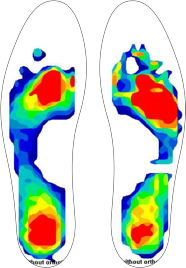
Affected Foot Scan F-Scan
In the case of hallux valgus deformity, function and power are significantly diminished under the big toe. Weight-bearing force is typically shifted laterally to the region under the second and third metatarsal heads. This lateral weight transfer is also accentuated by the collapse of the metatarsal arch in affected feet.