
Dear patients:
A bunion is not a growth, not a disease, not a fungus, and certainly nothing to be ashamed of. If you don’t have the condition, consider yourself lucky. If you do have it, you owe it to yourself to understand what’s going on.
While it’s one of the most common foot problems today, the condition is still not well understood, and therefore approaches to treatment, surgical correction in particular, are far from standardized. Doctors and online medical resources offer differing views because there is still no official consensus on the actual pathology, or specific reason for it's development. We believe this situation needs to change.

Validated by 35 years of successful outcomes, we offer a direct diagnosis, and therefore a true pathology.
What’s going on inside?
The word ‘bunion’ comes from the Greek word for turnip and is the common name for that annoying and sometimes painful protrusion on the side of your big toe joint. Medically, the condition is called a "hallux valgus" deformity, which means an outward tilting of the big toe. What you see on the surface, however, does not tell the whole story.
Doctors have long hypothesized different failure scenarios: “Is it the bones, joints, ligaments, muscles or tendons? What is the primary underlying reason for an otherwise anatomically normal foot to become so deformed later in life?” Simply put, the bones in the inner-side of your foot, or the medial column, have fallen apart.
The complex problem
The real culprits are incompetent ligaments. Drifting bones and joints are innocent bystanders. Displaced tendons and muscles only become accomplices after the fact.
This is a progressive condition that slowly reveal themselves over many years and through a complex sequence of events.
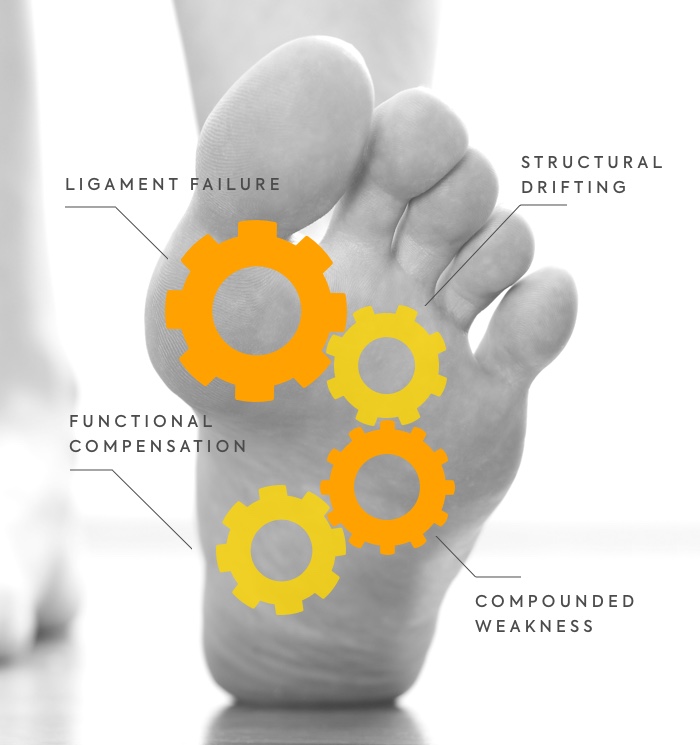
1. LIGAMENT FAILURE
A network of ligaments around the medial column begins to fail, particularly around the first metatarsal bone. Without this critical support, the bones in the medial column are allowed to drift apart.
2. STRUCTURAL DRIFTING
Under the stresses of daily activities, the first metatarsal’s head is slowly pushed away from the rest of the forefoot. At the top, the big toe caves in. The entire medial column rotates inward, and the sesamoid bones gradually drift outward.
3. COMPOUNDED WEAKNESS
A layered network of tendons and muscles connect the big toe to the rest of the foot. The tendon-embedded sesamoids act ingeniously as a pulley system to power big toe function. As the sesamoids dislocate, the entire medial column is rendered unstable and weak.
4. FUNCTIONAL COMPENSATION
When this critical walking mechanism is compromised, the foot naturally compensates. Weight-bearing force is transferred from the inner-side of the foot to the outer-side. The gait changes, and sooner or later secondary problems appear.
Indeed, this deformity is rarely a singular issue, and often cause secondary problems:
- Clawed & hammer toes
- Metatarsal calluses
- Collapsed longitudinal and transverse arches
- Metatarsalgia (pain under collapsed transverse arch)
- Morton’s neuroma
- Painful bunionettes
- Loss of balance
-
Low back, leg or knee pain
See Syndesmosis Surgery cases resolving secondary problems
80
GENETICS
80% of sufferers claim a family history of the same deformity.
What causes the ligaments to fail?
Nearly one quarter of the global adult female population suffer from the condition. Although high heels are infamously blamed, studies demonstrate these weakened ligaments are primarily related to the female estrogen hormone and heredity.
The female body has specifically evolved to be more flexible than the male body. During pregnancy, an increase in estrogen allows further loosening of the ligaments around pelvis to prepare for childbirth. This same hormone is also partly responsible for the loosening of ligaments in affected female feet.
Heredity also plays an important role, with 80% of sufferers claiming a family history of such deformity.
Furthermore, variable lifestyles contribute to the speed and severity by which the condition develops. High heels, pointed and tight shoes may precipitate an earlier onset and accelerate it's progression to vulnerable feet, but there is no evidence that high heels primarily cause hallux valgus deformities.
Other Myths
Can I prevent or stop this progression?

While it's too late to change your parents or gender that may be responsible for your current condition, you can minimize pain and maximize function through conservative measures. Surgery should only be a last resort.
- Pain management starts with choosing comfortable shoes. The most comfortable shoes are usually flatter, wider, roomier, softer, thick-soled and open-toed.
- Purpose-designed foot orthotics can help support the affected foot’s collapsing arches. They reduce metatarsal calluses, metatarsalgia, foot flatness, while increasing foot functionality and hopefully slowing progression.
- Regular physiotherapy and strengthening exercises may also help slow progression and help the big toe regain some lost function.
- Toe socks, spacers, splints and other apparatuses can help ease tightness and discomfort around the big toe joint.
- Anti-inflammatories, painkillers, ice, foot soaks and massage can help reduce swelling and soreness whenever necessary for temporary relief.